The University of California, the San Diego School of Medicine, describes a new method that uses machine learning to target disease targets and predicts whether a drug can obtain FDA approval. The findings of the study could drastically change how researchers sift through large amounts of data to obtain valuable information that is of great benefit to patients, the pharmaceutical industry, and national health care systems.
“This is primarily a drug that works perfectly on the preterm birth side that is similar or similar. This is a clinical case that is considered to be the Achilles' heel of any drug discovery system. ”
The availability of drugs, in the current situation, is costly and has a high level of attraction, which puts a lot of pressure on the industry to address this challenge. One area of high fall translates from pre-trial testing to clinical trials, where drugs that usually work well in inbred preclinical models, such as mice, do not translate into clinical patients, perhaps due to high variability and disease personality from one patient to another.
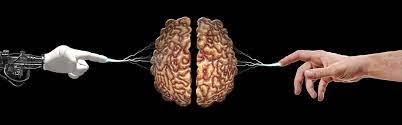
Now, researchers at the University of California San Diego, USA, led by Pradipta Ghosh, Soumita Das, and Debashis Sahoo have used a model of inflammatory bowel disease (IBD), using their two novel methods, instead of the first and last steps of drug discovery. before surgery. The first step called target identification used the artificial intelligence (AI) method that created a genetic map that extracted information that applied to all IBD patients and was used to find potential drug goals. The final step, called target validation for preoperative models, was performed for the first time in a Phase '0' clinical trial using a live biobank of organoids performed on IBD patients.
Researchers
have found that the use of computers has a surprisingly high level of accuracy
in various groups of IBD patients, and in line with Phase '0', they developed
the first-class treatment to restore and protect the leaky water barrier in
IBD.
The authors claim that the following steps include testing whether a drug that passed a '0 'human trial in a container can pass phase III tests at a clinic; and whether the same methods can be used with other diseases, from various cancers and Alzheimer's disease to non-alcoholic fatty acids.
"Our program has the potential to undermine the current situation and provide better treatment for chronic diseases that do not have the best treatment options," Ghosh said.
The approach could provide the predictive horsepower that will help doctors understand how diseases progress, assess a drug’s potential benefits and strategize how to use a combination of therapies when current treatment is failing.
Comments
Post a Comment